Our simple, minimally-invasive procedures target areas of arthritis and your injuries to relieve pain and restore function.*
*These statements have not been evaluated by the FDA. Innate healthcare Institute makes no claim to diagnose, treat, cure, or prevent any disease.
Success Stories
See what our patients say about our orthopedic and sports injury stem cell therapy:
“I thought it was a placebo effect at first. But within a few weeks, I was sleeping without pain, I have about 70% of motion back and I’m getting more and more active each week. In total, I’m about 80% pain-free. The treatment saved my career.”
– Bill R., Phoenix, AZ
“I’ve struggled with low back pain since my 20’s, I was a basketball player, had an accident and had surgery. Since then I’ve struggled with low back pain…I had to stop playing basketball, learned to walk again over 6 months. The pain got more and more frequent, it was a 10 out of 10 pain. I tried drugs…was offered to have another surgery but with having a son I couldn’t take 6 months off for recovery. Another doctor recommended I look into a stem cell procedure. I’ve been dealing with this pain for 20 years so I had nothing to lose. Since the treatment I noticed a change in 2 weeks, wasn’t having pain while trying to sleep, I’m working out 5 days a week with no pain. I have zero pain now. It’s been 8 months and the pain hasn’t come back. There was no time in a hospital. I’m getting stronger little by little with exercising.”
– Jenny R., Phoenix, AZ, Former College Basketball Star
“I had extreme pain in both knees, toes, and my thumb… my only option was surgery and I wanted an alternative so I could play with my grandkids. I didn’t want the recovery and downtime with the surgery. I had both my knees done and IV treatments with regenerative stem cell medicine. I don’t have any pain in my toes…I have no pain in my knees…I can play with my grandkids, go up and down hills… I’m back golfing 18 holes. I was at an 8/10 pain and now I have zero pain…no pain in the mornings, waking me up.”
– Deb S., Phoenix, AZ
“Being in the nursing field for over 50 yrs left me with bad knees and hips…I had a total knee replacement on left knee which went well. For my right knee I started researching other options and found stem cell medicine. I came in and had my right knee done and did really well, and my hips. My hips are well but not as well as my knee…the next day it was better…after a month there was no pain. I was bone on bone. The rehab from the knee replacement was very difficult. Now I workout 4 days a week, I continued to workout even after the stem cell injection. I do cardio classes and don’t have any pain in my knee during exercise, before I did…I’m much more functional and comfortable doing what I want to do…I think this is a great option to try before surgery…to me this makes 100% sense to do.”
– Marilyn Gardner, Phoenix, AZ

Changing the way we heal.
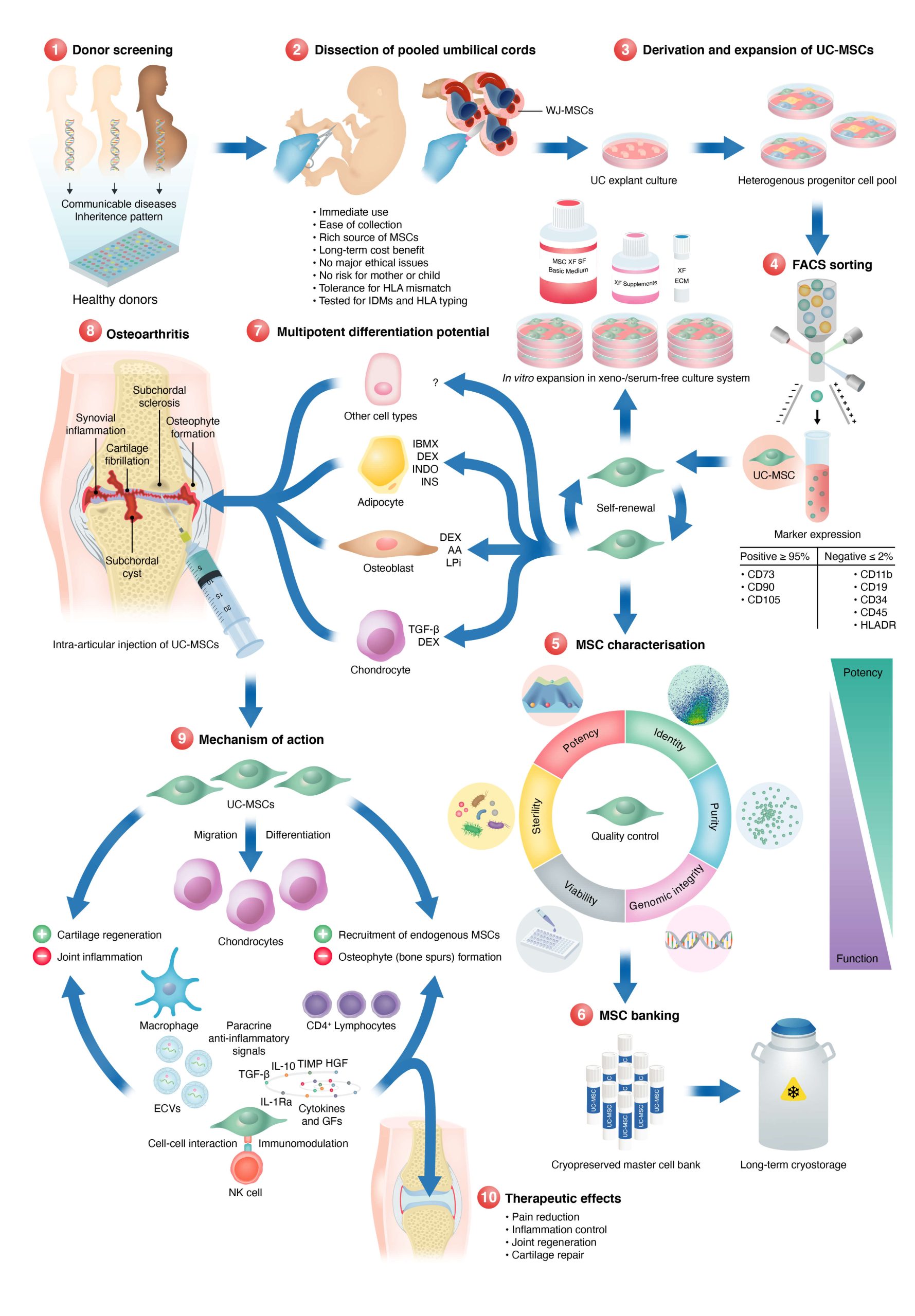
Umbilical Cord Mesenchymal Stem Cells are drastically changing our ability to treat diseases. In orthopedics and sports injuries these cells are transplanted to the site of injury to stimulate our bodies healing process. UC-MSCs can help heal damaged joints and injuries through multiple ways:
- Paracrine signaling (extracellular vesicles provide surrounding cells with growth factors, proteins, mRNAs, microRNAs, lipids, and DNA. These cells act as doctors distributing medicine to those cells in need.
- Increasing cell viability and proliferation (decrease the osteogenic genes (COX2, COL10A1 and MMP13)
- Suppressing inflammation –decreases production of inflammatory factors (TNF‐α, IL-1β, IL-6, IL-10)
- Inducing tissue repair and regeneration (promote chondrocyte proliferation)
- Improving angiogenesis (producing more blood vessels)
- Offering protection against osteoarthritis progression

The Research
Literature in the field of orthopedics with regenerative medicine such as umbilical cord stem cells, platelet-rich plasma, and prolotherapy have been ongoing for decades. Umbilical cord tissue has been defined as a very rich source for regenerative cells such as umbilical cord mesenchymal stem cells.
Studies have shown MSCs have the ability to migrate to sites of inflammation of injured tissue. MSCs release trophic factors (e.g. exosomes) at the site of injury and affect differentiation, angiogenesis (the creation of new blood vessels), and cytokine signaling. MSCs also repair tissue through potent immunosuppressive and anti-inflammatory interactions with our immune system. They literally change the cells in the injured environment to promote a healing environment.
A Systematic Review (meticulous summary of all the available primary research) was done on the effects of umbilical cord tissue mesenchymal stem cells would have on knee osteoarthritis (OA).
The researchers stated “Based on the results of this systematic review, many of the studies showed significant improvements following injection of UC-MSCs for the treatment of knee OA. Overall, the results illustrated positive clinical outcomes in the assessment of both pain and function at short-term follow-up. Furthermore, 3 studies included in this review evaluated the macroscopic ICRS score with all 3 reporting improvement in scores, indicating that UC-MSCs may actually repair cartilage damage from knee OA.”
Not only are UC-MSCs great at relieving pain after administration, they can significantly improve the function of the joint as well. A 2020 publication (Ann Transl Med 2021;9(6):452), a systematic review with conventional and network meta-analyses of randomized controlled trials, stated umbilical cord MSCs as the best source of stem cell treatments for functional improvement, compared to bone marrow and adipose stem cells. While all sources of MSCs showed improvements over placebo, the study reported UC-MSCs were considered to be the most effective cells for functional improvement (SMD =−1.02, 95% CI: −1.90 to −0.13, P=0.024) and that UC-MSCs have the largest probability of being the best treatment option for pain relief (SUCRA =85.3%).
How the cells are cultured/grown/handled is highly reflective of how well they can perform at healing, this is why it’s so imperative to find a clinic that is experienced in the field, and art, of regenerative medicine with umbilical cord tissue.
“Once kids started school in August I was out running about 3 miles every day. It was amazing and my body felt great. I stopped because… I found out I’m pregnant! I am so thankful for your clinic. It’s like I have been given a second chance at life. I feel better than I have in years.”

What To Expect
How it works
Umbilical cord mesenchymal stem cells and their exosomes have shown promise in healing arthritis and joint injuries due to their unique regenerative properties. These specialized cells possess the ability to differentiate into various cell types, including cartilage and bone cells, and can modulate the immune response and reduce inflammation. When introduced into the affected joint, these stem cells promote tissue repair by fostering the regeneration of damaged cartilage and inhibiting the inflammatory processes associated with arthritis. Additionally, they release bioactive molecules that stimulate the surrounding cells to contribute to the healing process. This multifaceted approach addresses both the structural damage and the underlying inflammatory component of arthritis, offering a potential therapeutic avenue for the treatment of joint injuries and degenerative conditions.
We we love it
Simply put, our regenerative techniques of utilizing umbilical cord mesenchymal stem cells can dramatically improve both pain and function due to damaged joints. Athletes can heal faster and better, return to their sport and play longer than before. Athletes benefit from this therapy over surgery as there is minimal downtime. Whereas most surgeries take months of downtime and rehabilitation, UC-MSC therapies have less significant downtime and athletes can return to their training and sport faster. Those that have been inactive due to pain can live more vibrantly and do things they haven’t done in years.
FAQs
Frequently Asked Questions
How do UC-MCs heal osteoarthritis?
Osteoarthritis is a degenerative joint disease that is characterized by the loss of cartilage, the tissue that cushions the joints. Umbilical cord mesenchymal stem cells (UC-MSCs) have been proposed as a potential therapeutic option for osteoarthritis due to their ability to differentiate into various types of cells, including chondrocytes (cartilage cells), and their ability to release various growth factors and other signaling molecules that can promote tissue repair and regeneration.
The process of how UC-MSCs may help to regenerate cartilage in osteoarthritis is not fully understood, but it is thought that they may work through a combination of different mechanisms, including:
- Chondrogenic differentiation: UC-MSCs can differentiate into chondrocytes, the cells that make up cartilage, which can help to repair and regenerate damaged or lost cartilage.
- Paracrine signaling: UC-MSCs can release various growth factors and other signaling molecules that can promote the proliferation and differentiation of chondrocytes, as well as the synthesis of extracellular matrix components, such as collagen and proteoglycans, which are essential for the formation and maintenance of cartilage.
- Anti-inflammatory effects: UC-MSCs can modulate the immune response, which can help to reduce inflammation in the joint, which can contribute to the development of osteoarthritis.
- Angiogenesis: UC-MSCs can also promote the formation of new blood vessels, which can help to supply oxygen and nutrients to the joint and support the repair and regeneration of cartilage.
Can UC-MSC be used to heal sports injuries and other tendon and ligament problems?
Tendons and ligaments are connective tissues that provide support and stability to joints and bones. Sports injuries, such as sprains and strains, can occur when these connective tissues are stretched or torn. Umbilical cord mesenchymal stem cells (UC-MSCs) have been proposed as a potential therapeutic option for these types of injuries due to their ability to differentiate into various types of cells, including fibroblasts (connective tissue cells), and their ability to release various growth factors and other signaling molecules that can promote tissue repair and regeneration.
Similar to other orthopedic problems, the process of how UC-MSCs may help to heal tendons and ligaments and sports injuries is not fully understood, but it is thought that they may work through a combination of different mechanisms, including:
- Fibroblast differentiation: UC-MSCs can differentiate into fibroblasts, the cells that make up tendons and ligaments, which can help to repair and regenerate damaged or lost connective tissue.
- Chondrogenic differentiation: UC-MSCs can differentiate into chondrocytes, the cells that make up cartilage, which can help to repair and regenerate damaged or lost cartilage.
- Paracrine signaling: UC-MSCs can release various growth factors and other signaling molecules that can promote the proliferation and differentiation of fibroblasts, as well as the synthesis of extracellular matrix components, such as collagen and proteoglycans, which are essential for the formation and maintenance of tendons and ligaments.
- Anti-inflammatory effects: UC-MSCs can modulate the immune response, which can help to reduce inflammation in the injured area, which can contribute to the healing process.
- Angiogenesis: UC-MSCs can also promote the formation of new blood vessels, which can help to supply oxygen and nutrients to the injured area and support the repair and regeneration of connective tissue.
What’s your stem cell process?
How are the UC-MSCs administered to address my painful joints?
Typically, a topical numbing agent will be applied. Followed shortly by a series of injections of dextrose prolotherapy. This is to help numb the area as well as give the doctor diagnostic feedback. This solution will also cause a low-grade inflammation to attract the cells healing properties. Unless noted otherwise, we will then draw your blood to prepare a regenerative solution called platelet-rich plasma (PRP). This PRP solution is then combined with the UC-MSCs and injected into the damaged tissue areas.
it is recommended to take at least two weeks of downtime after the procedure. This generally means no high-impact activity on the affected joint. This aftercare is different for all patients as their age, physical health, and lifestyle vary. this is an outpatient procedure in which the vast majority of patients travel to and from the clinic. Immobility, like that after surgery, is not required after orthopedic stem cell transplantation. Movement is encouraged after the procedure to promote the flow of blood to the treated area. This can be done with light activities such as swimming, yoga, physical therapy exercises, or even some light walking.
For those that are very adverse to needles, or worried that the procedure might be too painful for them, administration of light nitrous oxide sedation can be used.
How long have you been doing treatments for these conditions?
How long does it take to see results?
How long do the results last?
Do I need an MRI or Xray before treatment
Is sedation an option for orthopedic procedures?
Yes. We use a safe and effective light sedation system called Nitroseal. Nitrouseal® is a medical device that was invented by a Board-Certified Anesthesiologist specifically for administering nitrous sedation in any medical setting without exposing medical personnel to the exhaled nitrous. This is accomplished by utilizing a patented disposable face-mask and breathing circuit (tubing) to administer the inhaled nitrous/oxygen mixture and to then capture and eliminate the exhaled nitrous. The Nitrouseal® System has become the accepted standard for delivering nitrous sedation to kids in most pediatric hospitals nationwide.
Nitrouseal is a great option for our patients and offers a lot of benefits:
- Pain and anxiety relief.
- Extremely safe. Nitrous oxide has unparalleled safety record, is nonaddictive and opioid free.
- Flowmeter allows any concentration of nitrous 0% – 70%. You can individualize the dose to the patient and adjust up or down during the procedure.
- Very quick onset and very short duration (less than a minute). Patients can drive themselves home after.
- Self-administered by the patient and can be used for as long as the procedure lasts.
- Allows minor and minimally invasive procedures to be done in the office or at a medical facility while providing patient comfort.
How will I know what dose of UC-MSC is right for my condition?
Since UC-MSCs are safe we don’t have to worry about putting too many cells into a problem area, within reason. we’ve done complete whole body procedures without the 600 million cells with no adverse effects Except the obvious bruising, bleeding, and soreness from injection sites.
Some patients choose higher cell amounts to proactively treat their problem and make sure they get the best possible recovery. Using higher amounts of cells is encouraged since it allows for a higher probability of success. Since it’s your money and you’re paying for the treatments, we honor and value your feedback of what you want to do with your body. We will openly and transparently guide you if the dosage you want is too small for the problems you want addressed.
*These statements have not been evaluated by the FDA. Innate Healthcare Institute is a private clinic and any treatments utilizing any form of regenerative medicine is considered experimental.
Schedule a Consultation
Your next step is to schedule a consultation with our team. Click the button below to get started. If you prefer immediate assistance, please call us at 602-603-3118.
