FAQs
Frequently Asked Questions—
Orthopedic Treatments
*These statements have not been evaluated by the FDA. Innate Healthcare Institute is a private clinic and any treatments utilizing any form of regenerative medicine is considered experimental.
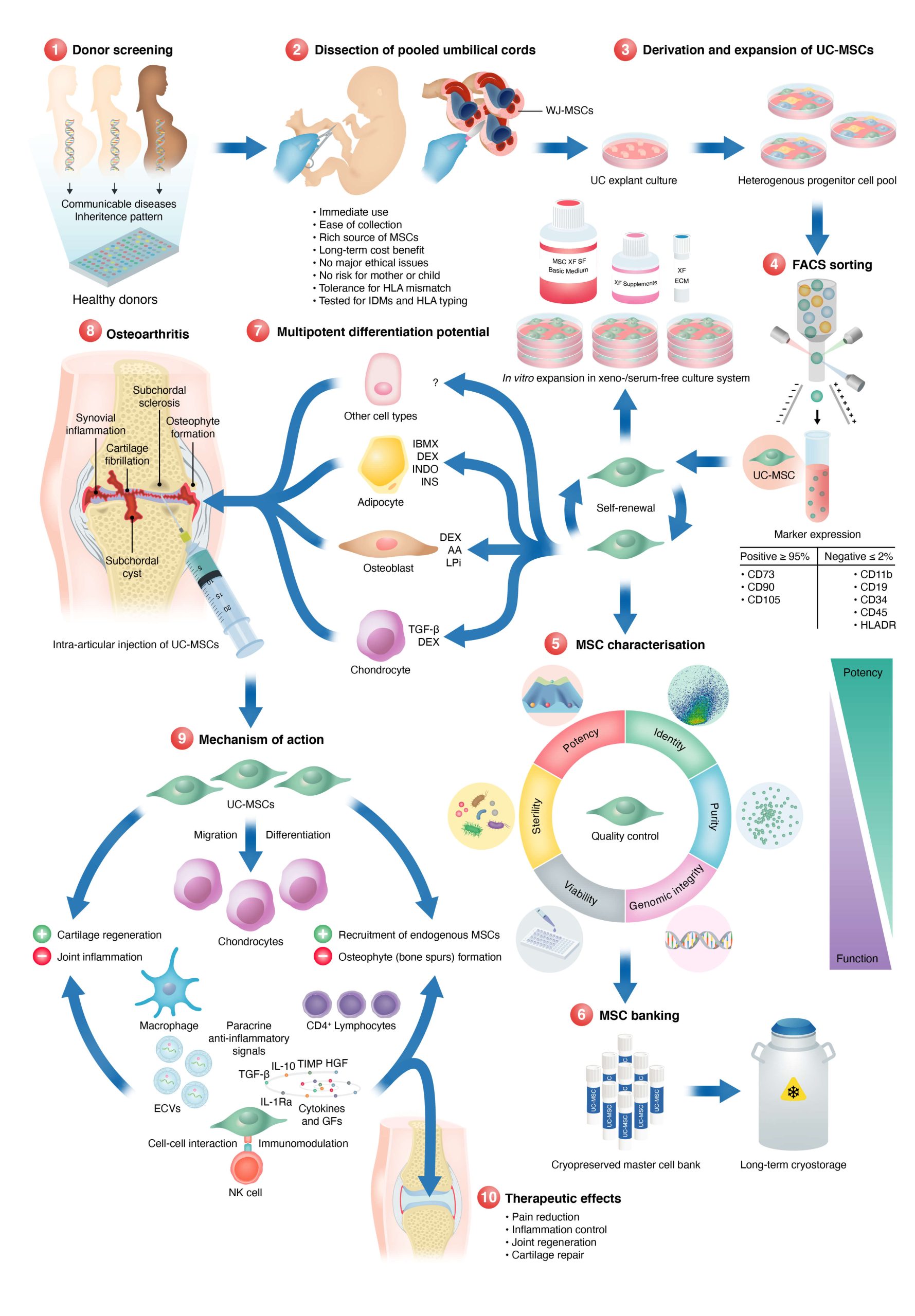
How do UC-MCs heal osteoarthritis?
Osteoarthritis is a degenerative joint disease that is characterized by the loss of cartilage, the tissue that cushions the joints. Umbilical cord mesenchymal stem cells (UC-MSCs) have been proposed as a potential therapeutic option for osteoarthritis due to their ability to differentiate into various types of cells, including chondrocytes (cartilage cells), and their ability to release various growth factors and other signaling molecules that can promote tissue repair and regeneration.
The process of how UC-MSCs may help to regenerate cartilage in osteoarthritis is not fully understood, but it is thought that they may work through a combination of different mechanisms, including:
- Chondrogenic differentiation: UC-MSCs can differentiate into chondrocytes, the cells that make up cartilage, which can help to repair and regenerate damaged or lost cartilage.
- Paracrine signaling: UC-MSCs can release various growth factors and other signaling molecules that can promote the proliferation and differentiation of chondrocytes, as well as the synthesis of extracellular matrix components, such as collagen and proteoglycans, which are essential for the formation and maintenance of cartilage.
- Anti-inflammatory effects: UC-MSCs can modulate the immune response, which can help to reduce inflammation in the joint, which can contribute to the development of osteoarthritis.
- Angiogenesis: UC-MSCs can also promote the formation of new blood vessels, which can help to supply oxygen and nutrients to the joint and support the repair and regeneration of cartilage.
Can UC-MSC be used to heal sports injuries and other tendon and ligament problems?
Tendons and ligaments are connective tissues that provide support and stability to joints and bones. Sports injuries, such as sprains and strains, can occur when these connective tissues are stretched or torn. Umbilical cord mesenchymal stem cells (UC-MSCs) have been proposed as a potential therapeutic option for these types of injuries due to their ability to differentiate into various types of cells, including fibroblasts (connective tissue cells), and their ability to release various growth factors and other signaling molecules that can promote tissue repair and regeneration.
Similar to other orthopedic problems, the process of how UC-MSCs may help to heal tendons and ligaments and sports injuries is not fully understood, but it is thought that they may work through a combination of different mechanisms, including:
- Fibroblast differentiation: UC-MSCs can differentiate into fibroblasts, the cells that make up tendons and ligaments, which can help to repair and regenerate damaged or lost connective tissue.
- Chondrogenic differentiation: UC-MSCs can differentiate into chondrocytes, the cells that make up cartilage, which can help to repair and regenerate damaged or lost cartilage.
- Paracrine signaling: UC-MSCs can release various growth factors and other signaling molecules that can promote the proliferation and differentiation of fibroblasts, as well as the synthesis of extracellular matrix components, such as collagen and proteoglycans, which are essential for the formation and maintenance of tendons and ligaments.
- Anti-inflammatory effects: UC-MSCs can modulate the immune response, which can help to reduce inflammation in the injured area, which can contribute to the healing process.
- Angiogenesis: UC-MSCs can also promote the formation of new blood vessels, which can help to supply oxygen and nutrients to the injured area and support the repair and regeneration of connective tissue.
What’s your stem cell process?
How are the UC-MSCs administered to address my painful joints?
Typically, a topical numbing agent will be applied. Followed shortly by a series of injections of dextrose prolotherapy. This is to help numb the area as well as give the doctor diagnostic feedback. This solution will also cause a low-grade inflammation to attract the cells healing properties. Unless noted otherwise, we will then draw your blood to prepare a regenerative solution called platelet-rich plasma (PRP). This PRP solution is then combined with the UC-MSCs and injected into the damaged tissue areas.
it is recommended to take at least two weeks of downtime after the procedure. This generally means no high-impact activity on the affected joint. This aftercare is different for all patients as their age, physical health, and lifestyle vary. this is an outpatient procedure in which the vast majority of patients travel to and from the clinic. Immobility, like that after surgery, is not required after orthopedic stem cell transplantation. Movement is encouraged after the procedure to promote the flow of blood to the treated area. This can be done with light activities such as swimming, yoga, physical therapy exercises, or even some light walking.
For those that are very adverse to needles, or worried that the procedure might be too painful for them, administration of light nitrous oxide sedation can be used.
How long have you been doing treatments for these conditions?
How long does it take to see results?
How long do the results last?
Do I need an MRI or Xray before treatment
Is sedation an option for orthopedic procedures?
Yes. We use a safe and effective light sedation system called Nitroseal. Nitrouseal® is a medical device that was invented by a Board-Certified Anesthesiologist specifically for administering nitrous sedation in any medical setting without exposing medical personnel to the exhaled nitrous. This is accomplished by utilizing a patented disposable face-mask and breathing circuit (tubing) to administer the inhaled nitrous/oxygen mixture and to then capture and eliminate the exhaled nitrous. The Nitrouseal® System has become the accepted standard for delivering nitrous sedation to kids in most pediatric hospitals nationwide.
Nitrouseal is a great option for our patients and offers a lot of benefits:
- Pain and anxiety relief.
- Extremely safe. Nitrous oxide has unparalleled safety record, is nonaddictive and opioid free.
- Flowmeter allows any concentration of nitrous 0% – 70%. You can individualize the dose to the patient and adjust up or down during the procedure.
- Very quick onset and very short duration (less than a minute). Patients can drive themselves home after.
- Self-administered by the patient and can be used for as long as the procedure lasts.
- Allows minor and minimally invasive procedures to be done in the office or at a medical facility while providing patient comfort.
How will I know what dose of UC-MSC is right for my condition?
Since UC-MSCs are very safe we don’t have to worry about putting too many cells into a problem area, within reason. We’ve used up to 600 million cells across multiple joints in one sitting with minor or no adverse effects. Some patients experience more inflammation after procedures than others, which can last for hours up to a few days on average. The obvious bruising, bleeding, and soreness from injection sites may occur as well.
Some patients choose higher cell amounts to proactively focus on their problem areas and make sure they get the best possible recovery. Using higher amounts of cells is encouraged since it allows for a higher probability of success and follows published research as well as clinical experience. Since it’s your money and you’re paying for the treatments, we honor and value your feedback on what you want to do with your body. We will openly and transparently guide you if the dosage you want is too small for the problems you want addressed.
We’d love to hear from you.
Don’t see your question? Click the button below to contact us. If you prefer immediate assistance, please call us at 602-603-3118.
